Navigating Insurance Credentialing: Tips for Faster Approvals
- TronsIT Solutions
- 0 Comments
Navigating Credentialing in the ever-evolving healthcare landscape of 2025 can feel like trying to solve a Rubik’s Cube blindfolded. But here’s the good news: it doesn’t have to be that way. Efficient navigation of insurance credentialing can significantly impact a practice’s operational efficiency and revenue cycle. This article provides updated strategies for 2025 to expedite approvals and streamline the credentialing process. Credentialing—it’s one of those behind-the-scenes processes that can either make or break your practice’s revenue cycle. In today’s fast-paced healthcare landscape, especially in 2025, efficient insurance credentialing isn’t just nice to have—it’s essential. Whether you’re a solo practitioner or managing a multi-provider clinic, faster credentialing means faster payments and smoother workflows.
Many practices are still stuck in outdated processes, resulting in costly delays. Let’s fix that.
Understanding Credentialing
Credentialing is the critical process healthcare providers must go through to verify their qualifications with insurance companies. It includes checking licenses, education, training, experience, malpractice history, and other certifications. In short, it’s the green light that allows providers to receive payments from insurers for treating patients.
According to a 2025 report by the American Medical Association, 82% of providers face delays in insurance reimbursements due to credentialing errors or incomplete submissions.
Why Is Credentialing So Time-Consuming?
Let’s look at some of the biggest bottlenecks:
Bottleneck | Description |
Incomplete Applications | Missing documents or outdated forms delay the entire process |
Varied Payer Requirements | Each insurer has unique criteria |
Manual Verification | Human errors and slow verifications waste weeks |
Poor Follow-up Systems | No consistent reminders or status checks |
Top 7 Powerful Tips to Speed Up Credentialing in 2025
Tip 1: Start Early and Stay Ahead
One of the golden rules in credentialing? Don’t wait until you’ve already hired the provider.
Start the credentialing process 60–90 days before the provider’s start date. Many insurance companies now allow pre-application and onboarding setups.
Pro tip: Create a credentialing checklist with all necessary documents and update it monthly.
Tip 2: Use Credentialing Software Tools
In 2025, automation is not a luxury; it’s a necessity.
Modern medical credentialing software platforms can:
- Auto-fill applications across multiple payers
- Alert you to missing or expiring documents
- Provide real-time tracking and status updates
Popular platforms include:
Platform | Key Features |
Medallion | Centralized dashboard, payer integration |
Verifiable | AI-powered compliance and verification |
CAQH ProView | Used by most major U.S. payers |
Tip 3: Don’t Skip the CAQH Profile
More than 90% of insurers in the U.S. require a CAQH (Council for Affordable Quality Healthcare) profile.
Make sure it’s:
- Updated with your most recent work history
- Free of typos
- Set to “authorize” for insurance companies to view
A locked or expired CAQH profile can delay your application by 4 to 6 weeks!
Tip 4: Assign a Credentialing Coordinator
With hybrid work models becoming the norm, employees should avoid using public Wi-Fi networks to access sensitive company data. Businesses should enforce the use of Virtual Private Networks (VPNs) and endpoint security solutions to protect remote workers.
4. Updating Software and Security Patches Regularly
Whether in-house or outsourced, having a dedicated person who manages your credentialing reduces errors, improves follow-ups, and ensures consistency.
In the middle of your process? This is where medical credentialing services can step in and take over. These experts are well-versed in payer protocols, reducing back-and-forth delays.
Tip 5: Follow Up Religiously
Once you submit your credentialing packet, the job isn’t over. Many delays happen because applications sit on someone’s desk.
Set a system of:
- Weekly check-ins with the payer
- Email confirmations for document receipt
- Log every interaction
Tip 6: Track License and Certification Expirations
Insurance panels often drop providers for having expired licenses or DEA certificates.
Create a renewal calendar that:
- Sends reminders 90/60/30 days in advance
- Automatically notifies HR and credentialing staff
Even better? Automated alerts via credentialing platforms.
Tip 7: Avoid Red Flags and Errors
Even one small mistake can restart the whole process. Watch for:
- Inconsistent job histories
- Incorrect NPI or license numbers
- Failing to disclose malpractice settlements
If in doubt, review documents three times before submission.

Credentialing Isn’t Just a Task—It’s a Strategy
Credentialing is more than paperwork. It’s your gateway to revenue. A delay in approval isn’t just frustrating—it can cost your practice tens of thousands of dollars in lost reimbursements.
That’s why a well-organized, proactive, and tech-savvy approach to credentialing can become your biggest asset.
And remember, when you outsource to a medical credentialing specialist, you’re not just getting a paper-pusher—you’re gaining a navigator who knows every shortcut.
Conclusion: Fast-Track Credentialing with TronsIT Solutions
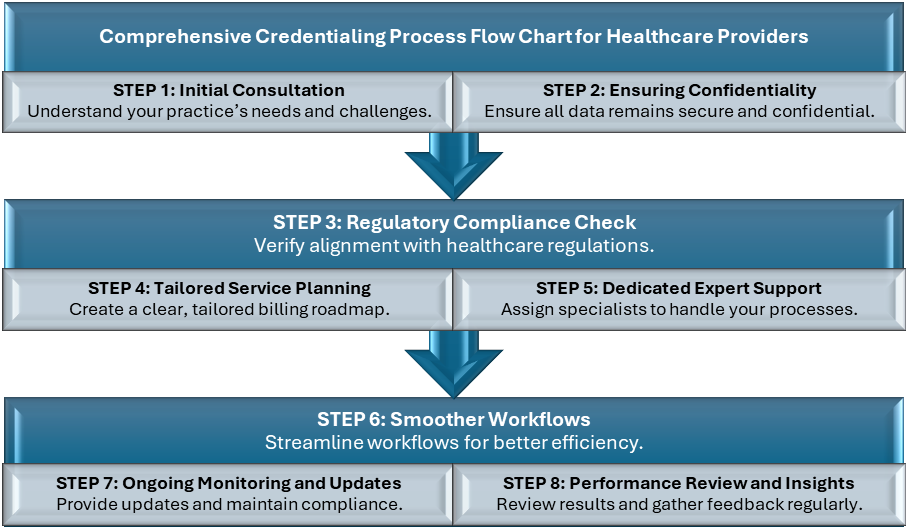
In 2025, navigating the maze of insurance approvals requires smart tools, strategic planning, and expert support. If you’re tired of delays and denials, TronsIT Solutions offers a streamlined approach to credentialing that blends technology with expertise.
With end-to-end credentialing services, automated workflows, and an expert team behind you, TronsIT Solutions makes it easy to get on panels, stay compliant, get paid fast and can reduce the time to approval by up to 40%.
TronsIT Solutions knows the ins and outs of:
- CAQH maintenance
- State licensing boards
- Insurance portal workflows
- PECOS and NPPES updates
- Credentialing audits and revalidations
For more informative blogs, explore our website!
Related Posts
Shaping the Future of KSA Healthcare with TronsIT Solutions
- TronsIT Solutions
- January 24, 2025
Healthcare is a central pillar of Saudi Arabia’s future vision, aiming to position the Ki ..
Medical Records for Sale? The Dark Reality of Healthcare
- TronsIT Solutions
- April 23, 2025
Introduction: The Rise and Risk of Electronic Health Records Electronic health records (EHRs) h ..



